ABSTRACT
This study aimed to examine nutrition care management for in-patients with dysphagia and to evaluate knowledge on nutrition care related to dysphagia among dietitians in clinical settings. A total of 554 questionnaires were distributed to dietitians at hospitals located in Seoul and Gyeonggi Province in Korea, and 147 responses were used for data analysis after excluding responses with significant missing data. Study participants worked at general hospitals (37.2%), long-term care hospitals (24.3%), hospitals (19.2%), and tertiary hospitals (11.5%). Prior education and training related to dysphagia was received by 69.9% of the respondents. The percentage of hospitals that had diet guidelines for dysphagia was 68.0%. Dysphagia diets of 2 levels and 3 levels were provided in 55.1% and 34.7% of the hospitals, respectively. Overall 74.7% of the dietitians responded that they provided information on dysphagia diets to in-patients and caregivers, but only 45.7% of dietitians did so in the long-term care hospitals. Among the respondents who used commercial thickening agents, 77.2% used only one type of commercial thickening agent. Patients or caregivers (75.7%) or nurses (34.5%) were reported to modify viscosity of liquid. Dietitians showed low levels of knowledge on nutrition care related to dysphagia (a mean of 5.14 based on possible scores from 0 to 10 points). To promote nutritional consumption and prevent malnutrition and aspiration, hospitals need the standardized diet guidelines, and dietitians should improve their expertise in nutritional care for patients with dysphagia.
-
Keywords: Dysphagia; Diet; Patients; Nutrition; Knowledge
INTRODUCTION
Dysphagia is defined as “anatomical or physiological abnormalities that interfere with swallowing [
1].” Dysphagia is most prevalent in the older population even though it can occur at any age [
2]. One systematic review reported that an estimated prevalence rate of dysphagia was 15% among older adults residing in the community [
3]. It was reported that 62.3% of Korean older adults living in the community were at risk of dysphagia [
4]. The prevalence rate increased in nursing home settings; 52.7% of residents in nursing homes had swallowing problems [
5]. In addition to old age, risk factors of dysphagia include institutionalization, reduced cognitive function, tube feeding, neuromuscular impairments, stroke history, and polypharmacy [
5]. In one study, 64% of the patients in the acute phase of stroke were found to have swallowing difficulties videofluoroscopically [
6].
If not detected early and treated properly, dysphagia may lead to such complications as malnutrition, dehydration, and aspiration pneumonia [
7]. Ekberg et al. [
8] found that over 50% of patients with dysphagia ate less, and 44% had experienced weight loss over the previous year. Decrease of food and liquid intakes among patients with dysphagia contributes to poor nutrition status [
9]. Stroke patients with dysphagia were 2.4 times more likely to be malnourished than those without dysphagia [
10]. In addition, stroke patients with dysphagia were hospitalized 2.5 times longer than those without dysphagia [
11]. While patients without swallowing difficulties were discharged home (76.9%), those with swallowing difficulties were discharged to rehabilitation centers (52.9%) and long-term care facilities (23.5%). Risk of aspiration, a complication of dysphagia, increased by 3-fold among stroke patients [
12]. Dysphagia also influences quality of life among patients. A multinational European survey revealed that 55% of patients with dysphagia enjoyed eating less, 41% experienced anxiety or panic during meals, and 36% avoided eating with others because of their dysphagia [
8].
Successful rehabilitation in patients with dysphagia is reported to reduce the prevalence of malnutrition and pneumonia [
7]. To improve safety and ease of oral intake and consumption of foods and liquids, diet modification is an essential part of dysphagia management [
13]. In addition to diet modification, postural adjustments and swallow maneuvers, and alternate nutrition strategies are also used for dysphagia management [
7]. Modified diets include texture-modified foods and thickened liquids that help patients to eat more comfortably and avoid aspiration. However, patients with dysphagia showed low acceptability and poor compliance with modified diets [
7]. Thickening agents negatively affect the flavor and texture of beverages, potentially making the thickened liquids less appetizing to patients [
14,
15]. While foods and liquids should be modified to the appropriate consistency for the patient's swallowing ability, it is reported that most healthcare staff were unable to correctly prepare modified liquids [
16]. As a result, many patients were served liquids that were incorrectly prepared and were placed at higher risk for aspiration pneumonia.
Dietitians on multidisciplinary teams for patients with dysphagia assess the nutritional needs of the patient, monitor the patient's consumption, plan meals suitable to the patient's dietary needs and swallowing abilities, and supervise foodservice staff who prepare meals [
13]. Once diet modifications have been made, dietitians should regularly evaluate and adjust diets according to the patient's changing condition. However, there are limited resources on diet management for Korean patients with dysphagia [
17], and degree of diet modifications vary from one setting to another. Although it is believed that professional nutrition service is important for dysphagia management, there are few reports on diet management of in-patients with dysphagia. The purposes of the study were to examine nutrition care management of in-patients with dysphagia and to evaluate knowledge on nutrition care for the patients among dietitians in clinical settings.
MATERIALS AND METHODS
Participants
Licensed dietitians were recruited from various types of hospitals based on classification by the Health Insurance Review and Assessment Service. A total of 554 questionnaires were distributed to dietitians working at tertiary hospitals, general hospitals, hospitals, and long-term care hospitals located in Seoul and Gyeonggi Province in Korea. A total of 151 responses were returned, and 147 responses were included in the data analysis after excluding responses with significant missing data.
Survey instrument and administration
A survey instrument was developed based on a review of the literature on nutrition management for patients in hospitals [
18,
19,
20,
21,
22,
23,
24] and was revised based on a review by clinical dietitians in hospitals. A final questionnaire consisted of 3 parts: profile of dietitians and hospitals, nutrition care services related to dysphagia, and knowledge on nutrition care for patients with dysphagia. Questionnaire items were also used to collect data on hospitals, including type of hospital, location, number of beds, and type of foodservice operation, and data on the dietitians, including work experience, educational background, and job duties. Availability of diet guidelines for dysphagia, provision of dysphagia diet, nutrition education/counseling, and modification of liquid viscosity were asked for nutrition care services for in-patients with dysphagia. Knowledge on nutrition care related to dysphagia among dietitians was assessed by 10 items for causes and symptoms of dysphagia, use of thickening agents, and meal management. For each correct answer, 1 point was given and the possible total score ranged from 0 to 10 points.
A packet including 1 questionnaire, 1 pre-paid return envelope, an informed consent form, and cover letter was mailed to dietitians working in the selected hospitals. The dietitians responded to the survey and returned it to the researchers by mail. The survey was performed from September 4 to September 29, 2017. The study proposal was approved by Seoul Women's University Institutional Review Board (IRB-2017A-18).
Statistical analysis
Descriptive statistics were calculated for all variables, and χ2 test and one-way analysis of variance (ANOVA) were performed to compare differences among variables collected by hospital and dietitian information. Duncan's post-hoc test was conducted when a significant difference was found from the ANOVA. All statistical analyses were performed using SPSS version 23.0 (IBM Corp., Armonk, NY, USA).
RESULTS
General characteristics of dietitians and hospitals
Among the 147 dietitians who participated in the survey, 37.2% worked in general hospitals and 24.3% worked in long-term care hospitals (
Table 1). Approximately 41% of dietitians had less than 5 years of working experience, and 20.6% had worked longer than 10 years. Of all the dietitians, 55.8% had a cook certificate and 42.2% had a clinical dietitian certificate. Prior education and training on dysphagia were received by 69.9% of the respondents, which were done from colleges/graduate schools (76.0%), academic associations (48.1%), Korean Dietetic Association (26.0%), and hospitals (23.1%).
Table 1General characteristics of respondents
Table 1
|
Variables |
Categories |
Frequency (%) |
|
Type of hospital |
Tertiary hospital |
17 (11.5) |
|
General hospital |
55 (37.2) |
|
Hospital |
27 (19.2) |
|
Long-term care hospital |
36 (24.3) |
|
Others |
12 (8.1) |
|
Working experiences, yr |
< 5 |
58 (41.1) |
|
5–10 |
54 (38.3) |
|
> 10 |
29 (20.6) |
|
Educational background |
Associate's degree |
40 (27.0) |
|
Bachelor's degree |
59 (39.9) |
|
Graduate degree |
46 (31.1) |
|
License/certificate*
|
Dietitian license |
146 (100.0) |
|
Cook certificate†
|
82 (55.8) |
|
Clinical dietitian certificate‡
|
62 (42.2) |
|
Certificate in nutrition for older adults§
|
8 (5.4) |
|
Certificate in foodservice management§
|
1 (0.7) |
|
Others |
7 (4.8) |
|
Major job duties |
Food service/clinical nutrition service |
91 (61.9) |
|
Food service management |
40 (27.2) |
|
Clinical nutrition service |
16 (10.8) |
|
Prior education/training on dysphagia |
Yes |
102 (69.9) |
|
No |
44 (30.1) |
|
Venues for prior education/training on dysphagia*
|
Undergraduate/postgraduate education |
79 (76.0) |
|
Academic association |
50 (48.1) |
|
Korean Dietetic Association |
27 (26.0) |
|
In-service education in hospitals |
13 (12.5) |
|
Education in other hospitals |
11 (10.6) |
|
Others |
3 (2.9) |
Nutrition care services for in-patients with dysphagia
Overall, 68% of the participants answered that their hospitals had diet guidelines for dysphagia (
Table 2). All tertiary hospitals and 83.6% of general hospitals had diet guidelines for dysphagia, whereas less than half of the hospitals and long-term care hospitals had the guidelines (p < 0.001). Dysphagia diets were provided by 100% of the tertiary hospitals, 96.4% of the general hospitals, 63.0% of the hospitals, and 61.1% of the long-term care hospitals (p < 0.001). More than half of the respondents (55.1%) responded that their hospitals provided dysphagia diets by 2 levels, and 34.7% answered that they provided diets by 3 levels. More than half of the tertiary hospitals provided dysphagia diets by 3 levels (52.9%), and 17.6% provided dysphagia diets by 4 levels. The majority of the hospitals (75.0%) and long-term care hospitals (68.2%) provided dysphagia diets by 2 levels (p < 0.05).
Table 2Nutrition care management for patients with dysphagia by hospital type
Table 2
|
Variables |
Categories |
Tertiary hospital (n = 17) |
General hospital (n = 55) |
Hospital (n = 27) |
Long-term care hospital (n = 36) |
Others (n = 12) |
Total (n = 147) |
p value |
|
Established guidelines for dysphagia diets |
Yes |
17 (100.0) |
46 (83.6) |
11 (40.7) |
17 (47.2) |
9 (75.0) |
100 (68.0) |
< 0.001 |
|
No |
0 (0.0) |
9 (16.4) |
16 (59.3) |
19 (52.8) |
3 (25.0) |
47 (32.0) |
|
Provision of dysphagia diets |
Yes |
17 (100.0) |
53 (96.4) |
17 (63.0) |
22 (61.1) |
10 (83.3) |
119 (81.0) |
< 0.001 |
|
No |
0 (0.0) |
2 (3.6) |
10 (37.0) |
14 (38.9) |
2 (16.7) |
28 (19.0) |
|
Stages of dysphagia diet |
1 level |
0 (0.0) |
2 (3.8) |
0 (0.0) |
3 (13.6) |
0 (0.0) |
5 (4.2) |
0.013 |
|
2 levels |
5 (29.4) |
24 (45.3) |
12 (75.0) |
15 (68.2) |
9 (90.0) |
65 (55.1) |
|
3 levels |
9 (52.9) |
24 (45.3) |
3 (18.8) |
4 (18.2) |
1 (10.0) |
41 (34.7) |
|
≥ 4 levels |
3 (17.6) |
3 (5.7) |
1 (6.3) |
0 (0.0) |
0 (0.0) |
7 (5.9) |
|
Explaining dysphagia to patients and caregivers |
Yes |
17 (100.0) |
50 (90.9) |
16 (59.3) |
16 (45.7) |
10 (97.0) |
109 (74.7) |
< 0.001 |
|
No |
0 (0.0) |
5 (9.1) |
11 (40.7) |
19 (54.3) |
2 (3.0) |
37 (25.3) |
|
Conducting nutrition counseling/education for patients and caregivers |
Yes |
10 (58.8) |
27 (49.1) |
6 (22.2) |
2 (5.6) |
1 (8.3) |
46 (31.3) |
< 0.001 |
|
No |
7 (41.2) |
28 (55.0) |
21 (77.8) |
34 (94.4) |
11 (91.7) |
101 (68.7) |
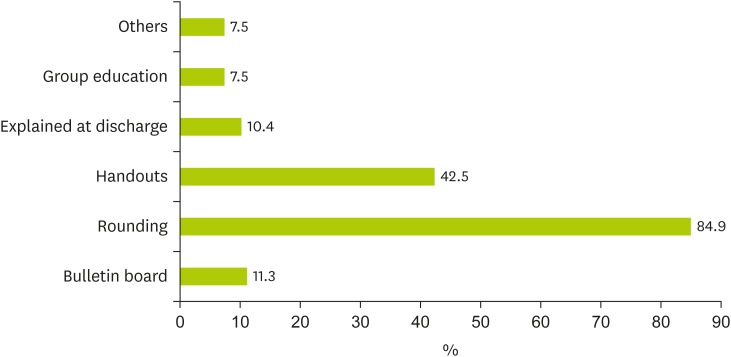
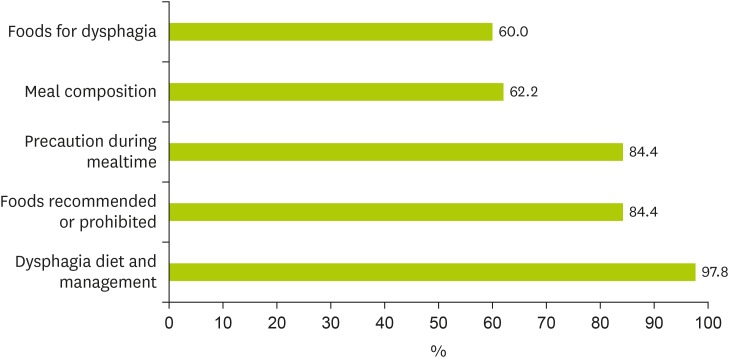
Overall, more than 70% of the dietitians answered that they provided information on dysphagia diets to in-patients and caregivers. All dietitians of tertiary hospitals answered that they had provided information on dysphagia diets to in-patients and caregivers, but only 45.7% of dietitians in the long-term care hospitals reported that they had (p < 0.001). The dietitians provided information on dysphagia through meal rounding (84.9%) and handouts (42.5%) (
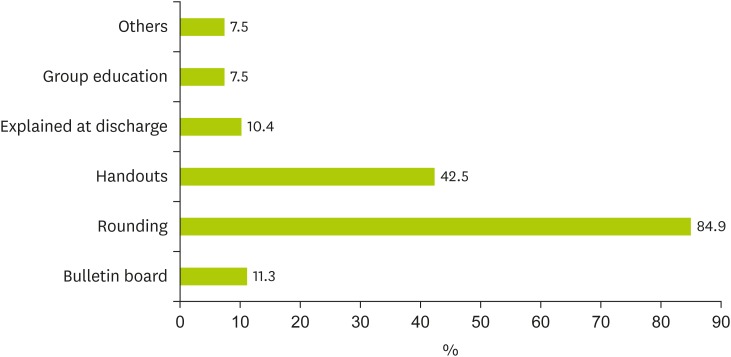
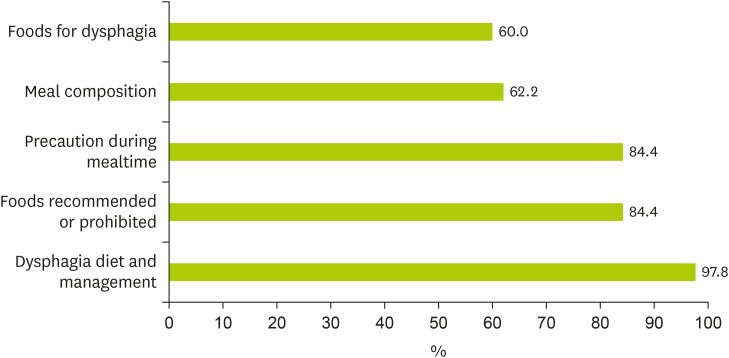
Figure 1). Nutrition counseling and education for patients and caregivers was delivered more in tertiary and general hospitals than in hospitals and long-term care hospitals (< 0.001). The subjects of the education/counseling included dysphagia diets and management (97.8%), foods allowed and prohibited (84.4%), and precaution during mealtime (84.4%) (
Figure 2).
Figure 1Methods for explaining dysphagia diets to patients and caregivers (multiple choices available).
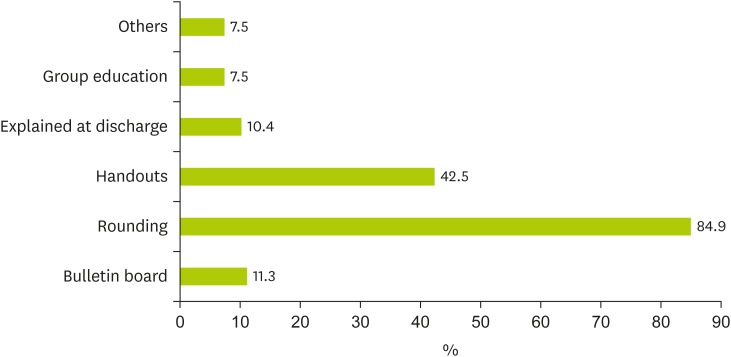
Figure 2Subjects for nutrition education for patients and caregivers (multiple choices available).
To modify viscosity of liquid, 65.8% of dietitians used commercial thickening agents (
Table 3). Among the dietitians who used commercial thickening agents, 77.2% used only 1 type of thickening agent. It was reported that no hospitals used 3 or more kinds of thickening agents. Most of the dietitians used xanthan gum-based thickening agents (49.2%) and mixed agents (43.7%) as commercial thickening agents. Viscosity of drinks was managed by patients or caregivers (75.7%) or nurses (34.5%).
Table 3Adjusting viscosity of liquid for dysphagia diet
Table 3
|
Variables |
Categories |
Frequency (%) |
|
Use of commercial thickeners |
Yes |
73 (65.8) |
|
No |
38 (34.2) |
|
No. of commercial thickeners used |
1 type |
44 (77.2) |
|
2 types |
13 (22.8) |
|
More than 3 types |
0 (0.0) |
|
Type(s) of thickener(s)*
|
Xanthan gum-based thickener |
35 (49.2) |
|
Mixed-based thickener |
31 (43.7) |
|
Guar gum-based thickener |
8 (11.3) |
|
Starch-based thickener |
6 (8.5) |
|
Person modifying viscosity liquid*
|
Patients/caregivers |
65 (75.7) |
|
Nurses |
39 (34.5) |
|
Cooks |
26 (23.0) |
|
Others |
17 (15.0) |
Dietitians’ knowledge on nutrition care for patients with dysphagia
A mean score of 5.14 ± 2.22 (based on 10 points) for the level of knowledge on nutrition care for patients with dysphagia indicated an overall lack of knowledge on the topic among dietitians (
Table 4). Most dietitians selected correct answers for identifying highest risk patients in dysphagia (73.5%) and eating posture of patients with tube feeding (60.5%). Less than 50% of the dietitians selected correct answers for causes of dysphagia (32.7%), characteristics of thickeners (42.9%), selecting proper foods for patients with dysphagia (45.6%), and symptoms of dysphagia (46.3%).
Table 4Dietitians’ knowledge on nutrition care for dysphagic patients
Table 4
|
Category |
Item |
Values*
|
|
Causes of dysphagia |
An 80-year-old man who is hospitalized with a pelvic fracture is more at risk for dysphagia than a 30-year-old pregnant woman or an 11-year-old girl with chronic allergies. |
108 (73.5) |
|
Cerebral infarction, liver cirrhosis, high blood pressure, and dementia cause dysphagia. |
48 (32.7) |
|
Signs of dysphagia |
When food enters the airways, patients with dysphagia will choke or cough. |
81 (55.1) |
|
Signs/symptoms of dysphagia include voice changes, coughing, and drooling. |
68 (46.3) |
|
Modified diet intervention |
The viscosity of water added with thickener does not change over time at room temperature. |
63 (42.9) |
|
When the same amount of thickener is added in the same amount of apple juice and water, the viscosity of the 2 beverages is the same. |
74 (50.3) |
|
Patients with dysphagia who can eat nectar-like foods can eat both plain yogurt and milk. |
67 (45.6) |
|
Patients with dysphagia who can eat pureed foods can also eat toast. |
82 (55.8) |
|
Feeding techniques |
An elderly patient fed by nasogastric tube can keep lying down during the feeding process. |
89 (60.5) |
|
It is safe for dysphagic patients to drink water while swallowing food. |
76 (51.7) |
|
Total score |
|
5.14 ± 2.22 |
The knowledge score on nutrition care for dysphagia was compared by dietitian’s general characteristics (
Table 5). The knowledge score of dietitians with working experience less than 5 years was significantly lower than that of dietitians with experience longer than 10 years (p < 0.05). Educational background also influenced the knowledge level. Dietitians with postgraduate degrees showed higher scores than those with associate degrees (p < 0.05). However, prior learning experience on dysphagia did not significantly affect the knowledge scores. Dietitians working at hospitals showed lower scores than those in tertiary or general hospitals (p < 0.01). There were no significant differences based on job duties.
Table 5Dietitians' knowledge on nutrition management for dysphagia patients by dietitian and hospital characteristics
Table 5
|
Classification |
Knowledge score |
p value |
|
Work experience, yr |
|
0.012 |
|
< 5 |
4.55 ± 1.93b
|
|
5–10 |
5.24 ± 1.97a,b
|
|
> 10 |
5.88 ± 2.63a
|
|
Education background |
|
0.049 |
|
Associate's degree |
4.48 ± 1.81b
|
|
Bachelor's degree |
5.14 ± 2.15a,b
|
|
Graduate degree |
5.65 ± 2.53a
|
|
Prior education/training on dysphagia |
|
0.074 |
|
Yes |
5.13 ± 2.35 |
|
No |
5.21 ± 1.95 |
|
Major job duties |
|
0.615 |
|
Food service management |
4.56 ± 1.74 |
|
Clinical nutrition service |
5.20 ± 2.01 |
|
Food service/clinical nutrition service |
5.43 ± 2.40 |
|
Type of hospital |
|
0.003 |
|
Tertiary hospital |
5.82 ± 2.43a,b
|
|
General hospital |
5.62 ± 2.42a,b
|
|
Hospital |
3.93 ± 1.80c
|
|
Long-term care hospital |
4.69 ± 1.75b,c
|
|
Others |
6.08 ± 1.98a
|
DISCUSSION
In this study, nutrition care services for in-patients with dysphagia and dietitians’ knowledge on nutrition care for patients with dysphagia were assessed in clinical settings. A total of 147 dietitians were surveyed from general hospitals (37.2%), long-term care hospitals (24.3%), hospitals (19.2%), and tertiary hospitals (11.5%). The proportion of hospitals that had established diet guidelines for dysphagia varied significantly by hospital type (p < 0.001): lower in the hospitals (40.7%) and long-term care hospitals (47.2%) than the tertiary (100%) and general hospitals (83.6%) (p < 0.001). A similar pattern was found for provision of dysphagia diets in the hospitals (p < 0.001). In this study, 61.1% of the long-term care hospitals provided dysphagia diets. This finding is similar to that of another study reporting that 63.1% of long-term care hospitals provided dysphagia diets [
22], but inconsistent with the finding of another study that reported that 31.6% of long-term care hospitals provided the diets [
20].
Overall, 68% of the hospitals had diet guidelines for dysphagia, and 81.0% provided dysphagia diets for in-patients. As a result, 19 hospitals (12.9%) provided dysphagia diets without formal diet guidelines. In Korea, standardized guidelines on dysphagia diets were not available at the time of the study, and most hospitals had developed and used their own guidelines, which resulted in inconsistent nutrition management for the patients with dysphagia across hospitals. Recently, a guide on food preparation for those with chewing and swallowing difficulties was developed [
17], but it has not yet been tested or adopted by healthcare professional associations. Policies on diet management affect nutrition care performance and cost of care for in-patients with dysphagia [
25]. Lee and Park [
20] reported that 46.6% of the dietitians in long-term care hospitals needed a standardized manual on clinical nutrition management to improve in this area.
To ensure that patients with dysphagia safely consume adequate nutrition, foods and liquids are modified according to health status, swallowing abilities, and compliance with the diets of individual patients. The majority of the hospitals are reported to provide dysphagia diets by 2 levels (55.1%) or 3 levels (34.7%). Some tertiary hospitals and general hospitals provided dysphagia diets by 4 levels (17.6% and 5.7%, respectively). Categorizing modified foods and liquids into the 4 levels was suggested by the National Dysphagia Diet Task Force [
23]. The categories include thin, nectar-like, honey-like, and spoon-thick. These distinctions are said to more adequately meet individual patient's specific needs. Although dysphagia is known to be more prevalent in long-term care facilities, 61.1% of the long-term care hospitals in this study provided dysphagia diets, and 68.2% of them offered diets by 2 levels. Prescriptions of thicknesses for modified diets vary among the skilled nursing facilities in the United States; an average of 8.3% of residents in skilled nursing facilities have received thickened liquids [
25]. However, there is no available data on the dysphagia diet levels provided in Korean hospitals.
An 1-level dysphagia diet was provided by 13.6% of the long-term care hospitals in this study. This finding indicates that patients may not be receiving a modified diet suitable for their swallowing status. Groher and McKaig [
26] reported that 31% of patients were offered modified diets, but only 5% of these patients were served an appropriate diet for their swallowing abilities in skilled nursing facilities. Some researchers addressed concerns that modified diets were not adjusted to a proper level as patients’ swallowing abilities changed [
7,
13]. It was reported that many patients with dysphagia remained at the same level for extended periods without reevaluation of their status in nursing homes [
26]. However, reevaluation of the residents' status revealed that 91% received a more restrictive diet than they needed. As swallowing abilities may be reversible or changed by swallow rehabilitation, their swallowing abilities and nutrition status should be monitored continuously and should be reflected on the diet [
13,
26].
Overall, 74.7% of the dietitians explained dysphagia diets to in-patients or caregivers. While 100% of the dietitians at tertiary hospitals explained dysphagia diet, less than half of dietitians at long-term care hospitals did so. This result is consistent with the past finding that explanation of therapeutic diet was provided in 38% of the long-term care hospitals [
27]. Nutrition counseling and education were delivered more frequently in tertiary and general hospitals than in hospitals and long-term care hospitals (p < 0.001). Similarly, group education for diabetes was provided more by tertiary hospitals compared with general hospitals and hospitals [
28]. It was reported that 57.5% of the in-patients with therapeutic diets had received nutrition counseling, and had positive perceptions regarding this service [
21]. In-patients admitted to tertiary and general hospitals reported that nutrition counseling would be helpful in maintaining health, improving dietary habits, and preventing diseases [
29].
Only 2 long-term care hospitals (5.6%) provided nutrition education for patients and their caregivers. The low performance level of nutrition care may be attributed to the lack of diet guidelines for dysphagia and poor staffing in the long-term care hospitals. It is reported that an average of 1.7 dietitians worked in a long-term care hospital but an average of 8.5 and 3.7 dietitians worked in a tertiary hospital and a general hospital, respectively [
27,
30]. Dietitians in long-term care hospitals were found to be more involved in production management (4.15/5.0) and safety/sanitation management (4.05/5.0) than nutrition management (1.65/5.0) [
31]. Dietitians should perform assessments of nutritional needs and status, monitor food and liquid intake, manage modified diets, and provide nutrition/counseling for patients/caregivers as a member of a multidisciplinary team for dysphagia management [
13]. While providing care for patients with dysphagia, dietitians manage foodservice and provide nutrition care services for other in-patients. Data show that 1 or 2 dietitians perform the work in hospitals and long-term care hospitals, which may decrease service levels and care quality for in-patients including dysphagia patients. Time for ongoing assessment and education/counseling for patients and caregivers should be considered in the staffing of dietitians at long-term care hospitals [
24]. Dietitians also reported a lack of awareness of the importance of nutrition management among other staff as a barrier toward conducting clinical nutrition services in long-term care settings [
20].
Because swallowing disorders can place patients at high risk for dehydration and aspiration, it is important to adjust the consistency of food and liquids according to the patient's swallowing abilities [
13]. Commercial thickening agents (65.8%) were frequently used for modifying viscosity of liquids in dysphagia diets. One type of commercial thickening agent was used by 77.2% of dietitians who used commercial thickening agents. Sura et al. [
7] indicated that compliance with thickened liquids was low among dysphagic patients and the low compliance led to reduced fluid intake and increased risk of dehydration. While starch-based thickeners show swallowing safety and efficiency [
32], they do not dissolve well, have starchy taste, and continue to thicken over time [
13,
33]. Gum-based thickeners reach target viscosity rapidly and maintain consistent viscosity over time but impart a slick texture [
34]. In this study, xanthan gum-based thickeners were used the most. Instead of using one type of thickener in a hospital, the use of thickeners should be based on the compliance needs of the individual patient [
15]. In many settings, liquids are thickened for patients with dysphagia; however, there is an argument that there was no evidence supporting the use of thickening agents for liquids [
7]. In addition to liquids, food texture is often modified in dysphagia diets; however, some foods that are a part of this diet, such as pureed foods, are not considered appetizing [
13,
15].
Elderly patients with cognitive or physical limitations such as dementia and stroke tend to depend on caregivers for eating. Feeding dependence increases risk for aspiration in patients with dysphagia when caregivers feed rapidly or improperly [
35]. In addition, the attitudes of nurses and other caregivers about patients’ diet can influence their consumption [
13]. In this study, modifying viscosity of drinks was managed primarily by patients or caregivers (44.2%) or nurses (26.5%). Preparing consistent thickened liquids to a standard is not easy [
13]. Dietitians should involve caregivers in diet management [
13] and provide caregivers with proper education/training on how to make thickened liquids and safe feeding.
Dietitians' knowledge on nutrition care for dysphagia was assessed as low (average score: 5.14/10.0). Only 32.7% of the dietitians correctly understood the causes of dysphagia, and only 46% correctly understood the signs and symptoms of dysphagia. The dietitians also showed lack of knowledge on diet modification, especially for use of thickening agents and selecting safe food for the patient. In this study, only 42.9% chose the correct response for the item “The viscosity of water added with thickener does not change over time at room temperature.” Similarly, one study found that most healthcare providers could not prepare modified liquids at the nectar- or honey-like thickness of liquids of the National Dysphagia Diet [
16]. Therefore, dietitians in clinical settings need to improve their knowledge on detecting symptoms of dysphagia and managing modified diets. In the survey, 30.1% of dietitians did not receive education related to dysphagia. Most respondents (76%) with prior education on dysphagia learned about dysphagia while attending college or graduate school. Continued learning opportunities that are related to current knowledge and evidence-based dysphagia management should be provided for dietitians by the Korean Dietetic Association and academic associations. The results of the study may not be generalized to all hospitals since the sample was selected in Seoul and Gyeonggi Province. The instrument for testing knowledge on dysphagia management has yet to be validated even though it was reviewed for its face validity by clinical dietitians. However, to the best of our knowledge, this study is the first report that focused on nutrition management practices for in-patients with dysphagia and included various hospital types in Korea. The data of the study will be useful for dietitians and other health professionals that provide care services for patients with dysphagia to improve care quality.
CONCLUSION
This study aimed to examine nutrition care practices for in-patients with dysphagia and to assess knowledge levels of dietitians on nutrition care of patients with dysphagia in clinical settings. A total of 147 dietitians participated in the survey from general hospitals (37.2%), long-term care hospitals (24.3%), hospitals (19.2%), and tertiary hospitals (11.5%). The proportion of hospitals that had established diet guidelines for dysphagia patients and provided dysphagia diets varied significantly by hospital type (p < 0.001). All tertiary hospitals and 83.6% of general hospitals had diet guidelines for dysphagia, whereas 63.0% of the hospitals and 61.1% of long-term care hospitals had (p < 0.001). Dysphagia diets were provided by 100% of the tertiary hospitals, 96.4% of the general hospitals, 63% of hospitals, and 61.1% of long-term care hospitals (p < 0.001). Overall, most hospitals provided 2-level or 3-level dysphagia diets (55.1% and 34.7%, respectively). It was also found that 17.6% of tertiary hospitals provided dysphagia diets by 4 levels, whereas 13.6% of long-term care hospitals provided dysphagia diets by 1 level (p < 0.001). Complications such as malnutrition and aspiration pneumonia may occur when modified diets do not match the patient’s nutritional requirements and swallowing abilities. To promote proper consumption and ensure safety, standardized diet guidelines that hospitals can use as a reference are needed.
Tertiary and general hospitals provided more explanation and nutrition education on dysphagia diets to patients and caregivers compared with long-term care hospitals and hospitals. The low level of nutrition care service in long-term care hospitals may be due to the lack of guidelines available for dysphagia and poor staffing. Among the dietitians that modified viscosity of liquids, most used commercial thickeners (65.8%) and 77.2% of these dietitians used only one type of thickener. Xanthan gum-based thickeners and mixed thickeners were used the most. Because the characteristics of thickeners vary by type, dietitians should take patient compliance with existing recommendations into consideration when determining which type of thickener to use. Texture-modified foods and liquids help patients with dysphagia consume foods and liquids safely. However, modification can make the food unappetizing and even dilute nutrient density. Modified diets are unlikely to match patients’ swallowing capabilities if their status is not re-assessed regularly. In this study, viscosity of liquid was modified by patients or caregivers (44.2%) or nurses (26.5%). Dietitians should involve caregivers in diet management and provide caregivers and other health professionals with education/training on how to make thickened liquids and safe feeding.
Dietitians showed low levels of knowledge on nutrition care for dysphagia patients. A low proportion of dietitians selected answers correctly for causes of dysphagia, signs/symptoms of dysphagia, use of thickeners, and appropriate foods for the patients. Only 69.9% of the dietitians had received prior education and training related to dysphagia. Continued learning opportunities that focus on causes and symptoms, diet modification, assessment, intervention, and monitoring of patients are needed for dietitians.
Seoul Women's University
NOTES
-
Funding: This work was supported by a research grant from Seoul Women's University (2019).
-
Conflict of Interest: The authors declare that they have no competing interests.
REFERENCES
- 1. Taylor KA, Barr SI. Provision of small, frequent meals does not improve energy intake of elderly residents with dysphagia who live in an extended-care facility. J Am Diet Assoc 2006;106:1115-1118.
- 2. Kawashima K, Motohashi Y, Fujishima I. Prevalence of dysphagia among community-dwelling elderly individuals as estimated using a questionnaire for dysphagia screening. Dysphagia 2004;19:266-271.
- 3. Madhavan A, LaGorio LA, Crary MA, Dahl WJ, Carnaby GD. Prevalence and risk factors for dysphagia in the community dwelling elderly: a systematic review. J Nutr Health Aging 2016;20:806-815.
- 4. Kim MS, Park YH. The risk of dysphagia and dysphagia-specific quality of life among community dwelling older adults in senior center. Korean J Adult Nurs 2014;26:393-402.
- 5. Park YH, Han HR, Oh BM, Lee J, Park JA, Yu SJ, Chang H. Prevalence and associated factors of dysphagia in nursing home residents. Geriatr Nurs 2013;34:212-217.
- 6. Mann G, Hankey GJ, Cameron D, Cameron D. Swallowing function after stroke: prognosis and prognostic factors at 6 months. Stroke 1999;30:744-748.
- 7. Sura L, Madhavan A, Carnaby G, Crary MA. Dysphagia in the elderly: management and nutritional considerations. Clin Interv Aging 2012;7:287-298.
- 8. Ekberg O, Hamdy S, Woisard V, Wuttge-Hannig A, Ortega P. Social and psychological burden of dysphagia: its impact on diagnosis and treatment. Dysphagia 2002;17:139-146.
- 9. Takeuchi K, Aida J, Ito K, Furuta M, Yamashita Y, Osaka K. Nutritional status and dysphagia risk among community-dwelling frail older adults. J Nutr Health Aging 2014;18:352-357.
- 10. Foley NC, Martin RE, Salter KL, Teasell RW. A review of the relationship between dysphagia and malnutrition following stroke. J Rehabil Med 2009;41:707-713.
- 11. Runions S, Rodrigue N, White C. Practice on an acute stroke unit after implementation of a decision-making algorithm for dietary management of dysphagia. J Neurosci Nurs 2004;36:200-207.
- 12. Martino R, Foley N, Bhogal S, Diamant N, Speechley M, Teasell R. Dysphagia after stroke: incidence, diagnosis, and pulmonary complications. Stroke 2005;36:2756-2763.
- 13. Garcia JM, Chambers E 4th. Managing dysphagia through diet modifications. Am J Nurs 2010;110:26-33.
- 14. Lotong V, Chun SS, Chambers E, Garcia JM. Texture and flavor characteristics of beverages containing commercial thickening agents for dysphagia diets. J Food Sci 2003;68:1537-1541.
- 15. Matta Z, Chambers E 4th, Mertz Garcia J, McGowan Helverson JM. Sensory characteristics of beverages prepared with commercial thickeners used for dysphagia diets. J Am Diet Assoc 2006;106:1049-1054.
- 16. Garcia JM, Chambers E 4th, Clark M, Helverson J, Matta Z. Quality of care issues for dysphagia: modifications involving oral fluids. J Clin Nurs 2010;19:1618-1624.
- 17. Korea Ministry of Food and Drug Safety. 2019 A guide to food preparation for people with difficulties in chewing and swallowing. Sejong: Korea Ministry of Food and Drug Safety; 2019.
- 18. Johnson S, Broady R, Marcus A, Touger-Decker R. Knowledge and performance of dysphagia risk screening among registered dietitians in clinical practice. Top Clin Nutr 2015;30:302-313.
- 19. Kim HJ, Kim EM, Kee GJ, Lee JJ, Lim JH, Lee JM, Leon HJ, Lee HY. Clinical nutrition service at medical centers in Seoul. J Korean Diet Assoc 2011;17:176-189.
- 20. Lee SJ, Park EJ. Importance-performance analysis of clinical nutrition management in convalescent hospitals in the Gyeongnam area. J Korean Diet Assoc 2016;22:53-69.
- 21. Yi JR, Son EJ, Lyu ES. Perception and satisfaction on nutrition counseling service for patients consuming a therapeutic diet at hospitals in Busan. J Korean Soc Food Sci Nutr 2010;39:1305-1312.
- 22. Park MS, Lyu ES. Importance and performance of dietitian’s task at long term care hospital foodservice in Busan·Kyungnam area. Korean J Community Nutr 2011;16:602-612.
- 23. McCallum SL. The national dysphagia diet: implementation at a regional rehabilitation center and hospital system. J Am Diet Assoc 2003;103:381-384.
- 24. Seo JS, Kim EM, Park MS, Son JM, Woo MH, Wie KA, Lee SM, Ju DL, Cha JA. Job standards and practice toolkits for clinical nutrition therapy: diabetes mellitus cancer dyslipidemia. Sejong: Ministry of Health & Welfare; 2014.
- 25. Castellanos VH, Butler E, Gluch L, Burke B. Use of thickened liquids in skilled nursing facilities. J Am Diet Assoc 2004;104:1222-1226.
- 26. Groher ME, McKaig TN. Dysphagia and dietary levels in skilled nursing facilities. J Am Geriatr Soc 1995;43:528-532.
- 27. Um MH, Lyu ES, Lee SM, Lee SM, Lee E, Cha JA, Park MS, Lee HS, Rha MY, Park YK. Clinical nutrition services of a long-term care hospital in Korea. Korean J Community Nutr 2015;20:220-235.
- 28. Kim HJ, Kim EM, Lee GJ, Lee JJ, Lim JH, Lee JM, Jeon HJ, Lee HY. Clinical nutrition service at medical centers in Seoul. J Korean Diet Assoc 2011;17:176-189.
- 29. Choi KB, Lee SM, Lee SM, Lee E, Park MS, Park YK, Cha JA, Lyu ES. Patient satisfaction and perception on nutritional counseling services quality. J Korean Soc Food Sci Nutr 2017;46:251-258.
- 30. Um MH, Park YK, Lee SO, Lee SM, Lee E, Cha JA, Park MS, Lee HS, Rha MY, Lyu ES. Clinical nutrition service in Korean tertiary hospitals and general hospitals: result of nationwide cross-sectional survey. J Korean Diet Assoc 2014;20:183-198.
- 31. Hong SY, Seo S. Job performance frequency and the training needs of dietitians in elderly healthcare facilities. J Korean Diet Assoc 2010;16:160-177.
- 32. Clavé P, de Kraa M, Arreola V, Girvent M, Farré R, Palomera E, Serra-Prat M. The effect of bolus viscosity on swallowing function in neurogenic dysphagia. Aliment Pharmacol Ther 2006;24:1385-1394.
- 33. Garcia JM, Chambers E 4th, Matta Z, Clark M. Viscosity measurements of nectar- and honey-thick liquids: product, liquid, and time comparisons. Dysphagia 2005;20:325-335.
- 34. Garcia JM, Chambers E 4th, Molander M. Thickened liquids: practice patterns of speech-language pathologists. Am J Speech Lang Pathol 2005;14:4-13.
- 35. Langmore SE, Terpenning MS, Schork A, Chen Y, Murray JT, Lopatin D, Loesche WJ. Predictors of aspiration pneumonia: how important is dysphagia? Dysphagia 1998;13:69-81.