ABSTRACT
This study was conducted to investigate the status of diabetes education in Korean diabetics and to analyze the association between blood sugar control and diabetes education. A total of 1,904 diabetic patients was classified into two groups (well-controlled group and uncontrolled group) using the 2008-2013 Korean National Health and Nutrition Survey data, and various variables were compared. Of the 1,904 patients, 15.9% had received diabetes education. The uncontrolled group had a low economic level, a high rate of drinking and obesity, and a low rate of moderate exercise. And the rate of drug treatment in the uncontrolled group was high, and the rate of education and nutrition education, and the total number of educations for diabetes were significantly lower than those in the control group. Factors affecting blood glucose control were analyzed drinking (odds ratio [OR], 1.34; 95% confidence interval [CI], 1.06–1.7), moderate exercise (OR, 0.45; 95% CI, 0.34–0.6), overweight and obesity (OR, 1.44; 95% CI, 1.17–1.78), duration of diagnosis (OR, 1.07; 95% CI, 1.05–1.08), treatment method (OR, 2.0; 95% CI, 1.45–2.77), nutritional education (OR, 0.62; 95% CI, 0.46–0.85), and education institution (OR, 0.71; 95% CI, 0.54–0.93). The results of this study support that education on lifestyle management, such as a balanced diet, regular exercise, and normal weight maintenance, is essential for blood glucose control, and patients with long-term treatment need cyclic and continuous education.
-
Keywords: Diabetes mellitus; Blood glucose; Educational status; Health communication
INTRODUCTION
The prevalence of diabetes is rapidly increasing worldwide [
1]. Diabetes itself is not only a cause of death, but complications also increase the medical costs and reduce the quality of life [
1,
2]. Hence, it is essential to prevent the occurrence of complications and delay the progress rate through proper diabetes management [
3]. Diabetes education is an important component after diagnosis, as managing diabetes requires self-management such as diet and exercise along with medication, and because education can acquire knowledge, skills and abilities [
4,
5]. Education has been reported to improve the patient's diabetes-related knowledge and self-care behavior, improve clinical indicators, including hemoglobin A1c (HbA1c), and lower the incidence of chronic complications [
6]. Education incurs costs, but consequently diabetes education has proven important by reporting cost-effectiveness [
7]. Diabetes education programs are common in individual counseling or group lectures, and education and public relations activities such as open lectures, camps, and meal experiences are also used. Recently, mobile-based application devices provide a variety of information [
8]. However, the most important aspect of diabetes education is the mutual trust between patients and educators, and the provision of accurate and professional information [
9]. To this end, domestic and foreign academic societies and related organizations are presenting data on new trends and strategic plans for diabetes education, and making various efforts, such as campaigns to improve awareness and dissemination of educational materials [
10].
Currently, diabetes education in Korea is being conducted through an education team consisting of doctors, nurses and clinical dietitians at hospitals. However, there is still a lack of systems and infrastructure, many patients do not use health care systems, and the patient's cognitive rate or control rate is still low. In addition, there is a lack of national research on diabetes education. The purpose of this study was to compare the conduct rate of education and needs according to the control status of diabetes patients using data from the Korea National Health and Nutrition Examination Survey and to analyze whether diabetes education affects blood sugar control.
MATERIALS AND METHODS
Subjects
This study used data from the 2008–2013 National Health and Nutrition Survey. Among the 53,829 subjects surveyed for a total of 6 years, those under 20 years of age (n = 13,046) and those without diabetes (n = 37,690) were excluded. 3,093 diabetes patients were first extracted. Subsequently, 1,904 subjects were extracted, excluding 1,189 subjects who included missing variables and inappropriate response data. The criteria for glucose control were classified into a well-controlled group (HbA1c < 6.5%, n = 585) and uncontrolled group (HbA1c ≥ 6.5%, n = 1,319).
Variables
All variables used in this study referred to the Korea National Health and Nutrition Survey Data guidelines. Demographic factors was investigated to sex (male, female), age (20–44 years, 45–64 years, and ≥ 65 years), economic level (low, middle-low, middle-high, and high), educational level (≤ middle school graduate, high school graduate and ≥ college graduate), occupation (white color, blue color and no occupation), national basic livelihood recipient (yes, no), marriage status I (single, married) and marriage status II (with spouse, without spouse and others). Lifestyle-related factors were confirmed quality of life (EQ5D index < 1, ≥ 1), stress level (too much, much, a little and almost never), alcohol drinking and smoking, exercise practice by intensity (hard, moderate and walking), usual sleeping time (< 7 hours, ≥ 7 hours), obese status (underweight, normal, overweight and obesity) and regularity of meals. Diabetes mellitus (DM)-related factors was analyzed to duration of diagnosis (≤ 1 year, 2 to 5 years, 6–10 years, 11–15 years, > 15 years), current treatment method of DM (insulin injection, oral medication, diet and/or exercise control and other methods), experience of nutritional education, education institution (clinics and hospitals, oriental medicine clinics, public health center, open lecture, workplace training, other places) and total numbers of educations.
Statistics
For all data, a complex sample analysis method was analyzed, using stratification, clusters, and step weights. The DM and education-related factors of the subjects were summarized in terms of mean and standard deviation for continuous variables and frequency and percentage (%) for categorical variables. Significant difference between well-controlled group and uncontrolled groups were identified by independent 2-sample t-test and Wilcoxon's rank-sum test in continuous data and Fisher's exact test in categorical data. Multivariate logistic regression analysis was also carried out to identify the factors that affect controlling of DM. Then it was visualized as a monogram. All analyses were carried out using R (version 3.6.1, The R Foundation for Statistical Computing, Vienna, Austria) and the statistical significance was set at 0.05 based on the 2-sided test.
RESULTS
Demographic factors in subjects
In the well-controlled group, the distribution of old age and national basic living recipients were significantly higher than in the uncontrolled group (
Table 1).
Table 1Demographic factors according to control status of blood glucose
Table 1
|
Variable |
Well-controlled (n = 585) |
Uncontrolled (n = 1,319) |
Total (n = 1,904) |
p value |
|
Sex |
|
|
|
0.243 |
|
Male |
298 (50.9) |
632 (47.9) |
930 (48.8) |
|
Female |
287 (49.1) |
687 (52.1) |
974 (51.2) |
|
Age (yr) |
|
|
|
< 0.001 |
|
20–44 |
30 (5.1) |
55 (4.2) |
85 (4.4) |
|
45–64 |
213 (36.4) |
620 (47.0) |
833 (43.8) |
|
≥ 65 |
342 (58.5) |
644 (48.8) |
986 (51.8) |
|
Economic level |
|
|
|
< 0.001 |
|
Low |
267 (45.6) |
447 (33.9) |
714 (37.5) |
|
Middle-low |
137 (23.4) |
366 (27.7) |
503 (26.4) |
|
Middle-high |
88 (15.1) |
273 (20.7) |
361 (19.0) |
|
High |
93 (15.9) |
233 (17.7) |
326 (17.1) |
|
Educational level |
|
|
|
0.117 |
|
≤ Middle school graduate |
405 (69.2) |
867 (65.7) |
1,272 (66.8) |
|
High school graduate |
110 (18.8) |
304 (23.0) |
414 (21.8) |
|
≥ College graduate |
70 (12.0) |
148 (11.2) |
218 (11.4) |
|
Occupation |
|
|
|
0.031 |
|
White color |
70 (12.0) |
218 (16.5) |
288 (15.2) |
|
Blue color |
170 (29.0) |
381 (28.9) |
551 (28.9) |
|
No occupation |
345 (59.0) |
720 (54.6) |
1,065 (55.9) |
|
National basic livelihood recipient |
|
|
|
0.004 |
|
No |
512 (87.5) |
1,212 (91.9) |
1,724 (90.5) |
|
Yes |
73 (12.5) |
107 (8.1) |
180 (9.5) |
|
Marriage status I |
|
|
|
1.000 |
|
Single |
10 (1.7) |
24 (1.8) |
34 (1.8) |
|
Married |
575 (98.3) |
1,295 (98.2) |
1,870 (98.2) |
|
Marriage status II |
|
|
|
0.395 |
|
With spouse |
435 (74.4) |
1,015 (77.0) |
1,450 (76.2) |
|
Without spouse |
140 (23.9) |
279 (21.1) |
419 (22.0) |
|
Others (Single) |
10 (1.7) |
25 (1.9) |
35 (1.8) |
Comparison of lifestyle-related factors in subjects
Among the total subjects, 47.2% showed a good quality of life of 1 point or higher, and 76% of all subjects had little or no stress, and there was no difference between the 2 groups. The drinking rate was 77.4% in the uncontrolled group, significantly higher than in the 69.7% in the well-controlled group, and the regular exercise rate of the moderate exercise was 19.0% in the well-controlled group and 9.6% in the uncontrolled group, and there were significant differences between the 2 groups. In the degree of obesity, the well-controlled group was 59.8% in normal, 38.3% in overweight and obesity. The uncontrolled group was 52.2% in normal, and 45.9% in overweight and obesity (
Table 2).
Table 2Lifestyle-related factors according to control status of blood glucose
Table 2
|
Variable |
Well-controlled (n = 585) |
Uncontrolled (n = 1,319) |
Total (n = 1,904) |
p value |
|
EQ5D index |
|
|
|
0.524 |
|
< 1 |
316 (54.0) |
690 (52.3) |
1,006 (52.8) |
|
≥ 1 |
269 (46.0) |
629 (47.7) |
898 (47.2) |
|
Stress level |
|
|
|
0.564 |
|
Too much |
29 (5.0) |
68 (5.2) |
97 (5.1) |
|
Much |
116 (19.8) |
243 (18.4) |
359 (18.9) |
|
A little |
301 (51.4) |
656 (49.7) |
957 (50.3) |
|
Almost never |
139 (23.8) |
352 (26.7) |
491 (25.7) |
|
Alcohol drinking |
408 (69.7) |
1,021 (77.4) |
1,429 (75.1) |
< 0.001 |
|
Smoking |
95 (16.2) |
253 (19.2) |
348 (18.3) |
0.142 |
|
Hard exercise |
83 (14.2) |
159 (12.1) |
242 (12.7) |
0.224 |
|
Moderate exercise |
111 (19.0) |
127 (9.6) |
238 (12.5) |
< 0.001 |
|
Walking |
255 (43.6) |
560 (42.5) |
815 (42.8) |
0.681 |
|
Sleep time (hr) |
|
|
|
0.375 |
|
< 7 |
269 (46.0) |
576 (43.7) |
845 (44.4) |
|
≥ 7 |
316 (54.0) |
743 (56.3) |
1,059 (55.6) |
|
Obesity |
|
|
|
0.007 |
|
Underweight |
11 (1.9) |
25 (1.9) |
36 (1.9) |
|
Normal |
350 (59.8) |
688 (52.2) |
1,038 (54.5) |
|
Overweight and obesity |
224 (38.3) |
606 (45.9) |
830 (43.6) |
|
Regularity of meal |
|
|
|
|
|
Breakfast |
518 (88.5) |
1,211 (91.8) |
1,729 (90.8) |
0.029 |
|
Lunch |
542 (92.6) |
1,240 (94.0) |
1,782 (93.6) |
0.309 |
|
Dinner |
556 (95.0) |
1,265 (95.9) |
1,821 (95.6) |
0.466 |
Comparison of DM-related factors in subjects
Diabetes diagnosis period was significantly shorter in the well-controlled group than in the uncontrolled group. The proportion of respondents who said they were treating for diabetes was 84.6% in the well-controlled group and 92.6% in the uncontrolled group. As a treatment method, the ratio of insulin injection and use of oral medication in the uncontrolled group was significantly high. In the subjects, the experience rate of nutritional education was 14.4% in the well-controlled group and 10.2% in the uncontrolled group. As for the institution of receiving education, there was a significant difference in 8.9% of hospitals in the well-controlled group, 7.2% in various open lectures, 5.1% in public health centers. The total number of educations showed significant difference in 0.28 times in the well-controlled group and 0.15 times in the uncontrolled group (
Table 3).
Table 3DM-related factors according to control status of blood glucose
Table 3
|
Variable |
Well-controlled (n = 585) |
Uncontrolled (n = 1,319) |
Total (n = 1,904) |
p value |
|
Duration of diagnosis of DM (year) |
|
|
|
< 0.001 |
|
≤ 1 |
126 (21.5) |
158 (12.0) |
284 (14.9) |
|
2–5 |
180 (30.8) |
280 (21.2) |
460 (24.2) |
|
6–10 |
143 (24.4) |
312 (23.7) |
455 (23.9) |
|
11–15 |
66 (11.3) |
249 (18.9) |
315 (16.5) |
|
> 15 |
70 (12.0) |
320 (24.2) |
390 (20.5) |
|
Treatment method of DM |
495 (84.6) |
1,222 (92.6) |
1,717 (90.2) |
< 0.001 |
|
Insulin injection |
16 (2.7) |
150 (11.4) |
166 (8.7) |
< 0.001 |
|
Oral medication |
470 (80.3) |
1,157 (87.7) |
1,627 (85.5) |
< 0.001 |
|
Diet and/or exercise control |
128 (21.9) |
328 (24.9) |
456 (23.9) |
0.177 |
|
Other method (remedy and etc on) |
2 (0.3) |
3 (0.2) |
5 (0.3) |
1.000 |
|
Nutritional education |
84 (14.4) |
134 (10.2) |
218 (11.4) |
0.010 |
|
Education institution |
118 (20.2) |
185 (14.0) |
303 (15.9) |
0.001 |
|
Clinics and hospitals |
52 (8.9) |
69 (5.2) |
121 (6.4) |
0.004 |
|
Oriental medicine clinics |
12 (2.1) |
34 (2.7) |
46 (2.4) |
0.597 |
|
Public health center |
30 (5.1) |
15 (1.1) |
45 (2.4) |
< 0.001 |
|
Open lecture |
42 (7.3) |
66 (5.0) |
108 (5.6) |
0.074 |
|
Workplace training |
16 (2.7) |
0 (0.0) |
16 (0.8) |
< 0.001 |
|
Other places |
11 (1.9) |
15 (1.1) |
26 (1.4) |
0.282 |
|
Total No. of educations |
0.28 ± 0.74 |
0.15 ± 0.41 |
0.19 ± 0.54 |
< 0.001 |
Factors affecting glucose control
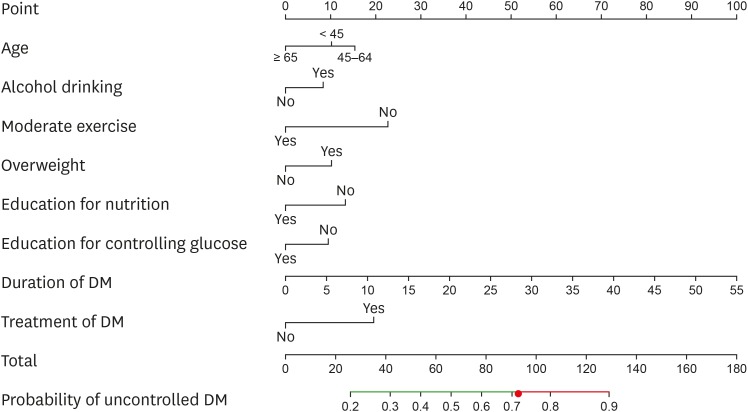
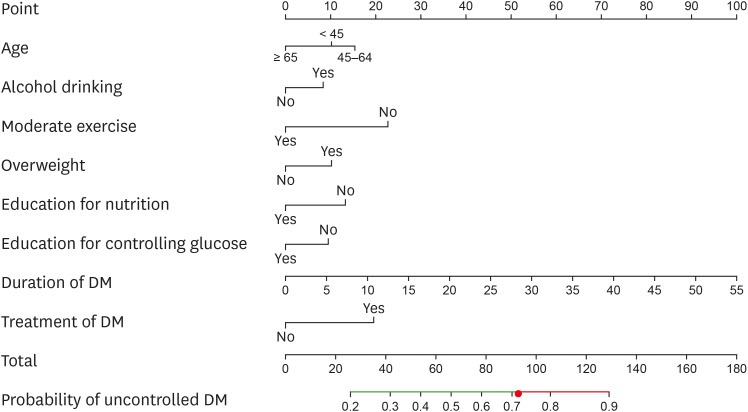
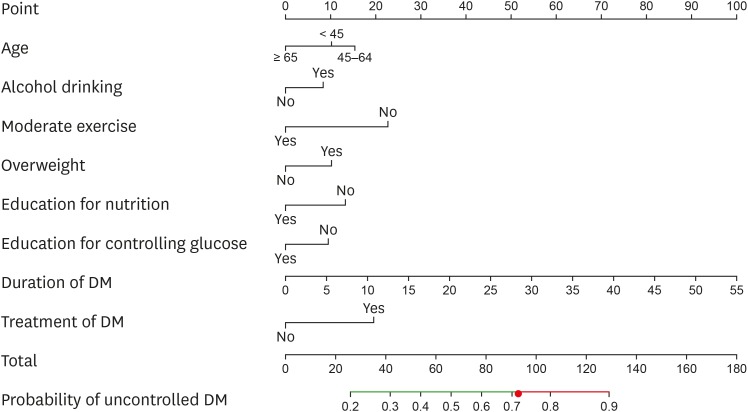
Table 4 shows the analysis results of factors affecting glucose control through various variables of the subjects. As a result of performing multiple logistic regression by recalibrating the significant factors through a univariate analysis, the significant factors were analyzed drinking (odds ratio [OR], 1.34; 95% confidence interval [CI], 1.06–1.70), moderate exercise (OR, 0.45; 95% CI, 0.34–0.60), overweight and obesity (OR, 1.44; 95% CI, 1.17–1.78), duration of diagnosis (OR, 1.07; 95% CI, 1.05–1.08), treatment method (OR, 2.0; 95% CI, 1.45–2.77), nutritional education (OR, 0.62; 95% CI, 0.46–0.85), and education institution (OR, 0.71; 95% CI, 0.54–0.93). The results of the monogram representation of the regression analysis results are shown in
Figure 1. If the sum of points for each variable is higher than the cutoff value of 0.714, it is confirmed that glucose is not controlled (
Table 3 and
Figure 1).
Table 4Logistic regression analysis for control status of blood glucose
Table 4
|
Variable |
Univariable |
Multivariable |
|
OR (95% CI) |
p value |
OR (95% CI) |
p value |
|
Demographic factor |
|
|
|
|
|
Age 45–65 (vs. 19–44) |
1.59 (0.99–2.54) |
0.055 |
1.20 (0.73–1.97) |
0.468 |
|
Age ≥ 65 (vs. 19–44) |
1.03 (0.65–1.63) |
0.910 |
0.70 (0.43–1.14) |
0.151 |
|
Middle-low income (vs. low) |
1.60 (1.25–2.04) |
< 0.001 |
- |
- |
|
Middle-high income (vs. low) |
1.85 (1.39–2.46) |
< 0.001 |
- |
- |
|
High income (vs. low) |
1.50 (1.13–1.99) |
0.005 |
- |
- |
|
White color (vs. No occupation) |
1.49 (1.11–2.01) |
0.009 |
- |
- |
|
Blue color (vs. No occupation) |
1.07 (0.86–1.34) |
0.529 |
- |
- |
|
National basic livelihood recipient |
0.62 (0.45–0.85) |
0.003 |
- |
- |
|
Lifestyle-related factor |
|
|
|
|
|
Alcohol drinking |
1.49 (1.19–1.85) |
< 0.001 |
1.34 (1.06–1.70) |
0.014 |
|
Moderate exercise |
0.45 (0.35–0.60) |
< 0.001 |
0.45 (0.34–0.60) |
< 0.001 |
|
Overweight and obesity |
1.37 (1.12–1.67) |
0.002 |
1.44 (1.17–1.78) |
< 0.001 |
|
Having breakfast |
1.45 (1.05–2.00) |
0.024 |
- |
- |
|
DM-related factor |
|
|
|
|
|
Duration of diagnosis of DM (yr) |
1.06 (1.04–1.08) |
< 0.001 |
1.07 (1.05–1.08) |
< 0.001 |
|
Treatment method of DM |
2.29 (1.69–3.11) |
< 0.001 |
2.00 (1.45–2.77) |
< 0.001 |
|
Nutritional education |
0.67 (0.50–0.90) |
0.008 |
0.62 (0.46–0.85) |
0.003 |
|
Education institution |
0.65 (0.50–0.83) |
< 0.001 |
0.71 (0.54–0.93) |
0.013 |
Figure 1
Nomogram for predicting the uncontrolled glucose in patients with DM.
Instruction for using the nomogram is as follows. First, draw a straight upward line to ‘Point’ axis and determine the points contributed by age. In this case, the subjects aged 45 to 64 contributes to 14 points, while being aged below 45 and over 65 contributes to 10 and 0 points, respectively. Second, repeat the same process for alcohol drinking, moderate exercise, overweight, education for nutrition or controlling glucose, duration of DM, and treatment of DM. Third, add up all the points from the 8 domains to get total points. Last, draw a straight downward line from the ‘Total’ axis to the ‘Probability of uncontrolled DM’ axis and get the estimated probability. The probability of greater than 0.714 was determined as the patient un-controlling glucose. The cutoff value of 0.714 was computed by Youden's index.
DM, diabetes mellitus.
DISCUSSION
Diabetes education has been important both treatment and prevention, and patients themselves must have sufficient knowledge of diabetes for success of treatment [
11]. In the previous study, it was found that patients with diabetes education had higher knowledge and better glucose control than patients without education [
12]. In this study, we tried to confirm again the importance of diabetes education through national big data analysis based on several reports that the control rate is very low compared to the awareness rate of diabetic patients in Korea and the education performance rate is still low. As a result of analysis, the uncontrolled group had a relatively young age group and a significantly higher proportion of the white-color occupational group. Diabetes patients in Korean, the age of diagnosis is getting lower, and this is related to the increase in insulin resistance and the increase in obesity due to the westernization of diet and decreased activity [
13]. In addition, the uncontrolled group showed a higher rate of drinking, a lower rate of moderate exercise, and a higher rate of obesity. These results suggest that more dietary control and exercise practice need to be aggressively involved, considering the results of a prior study in which exercise and dietary control have a significant effect on blood sugar in managing diabetes [
14,
15].
In the result of analysis of factors related to diabetes, the uncontrolled group had a relatively long diagnosis duration and a high rate of drug treatment, but the rate of nutrition education and the total number of educations were found to be significantly lower. Having analyzed the factors affecting glucose control, it was found that drinking, overweight and obesity, diabetes diagnosis duration and treatment status had a negative effect on glucose control, and nutrition education and education place had a positive effect. Diabetes is important for dietary management, but it is one of the most difficult practices for many patients, and medications ordered by doctors are continued, but nutrition education is often avoided [
16]. However, there have been many studies that showed that patients with diabetes nutrition education have not only altered nutrient intake but also increased nutritional knowledge and showed desirable eating behaviors [
17,
18]. Furthermore, the need for more systematic counseling and dietary adjustment has been steadily proposed to manage for a long time and prevent complications, and educators in various fields should cooperate to induce patient changes [
19]. Diabetes is known to be more effective in improving glucose levels as the number of education interventions increases, and regular and frequent education programs are known to help self-management [
20]. There was also a study that confirmed that the intervention group had increased self-care and self-efficacy compared to the control group when education for 12 weeks was provided to patients with type 2 diabetes once a week for a total of 12 weeks [
21]. This study is a retrospective study, so it is not possible to confirm the clinical outcome depending on the content, method, and frequency of education, but education must be performed on patients diagnosed with diabetes as the educational experience and frequency of education in the uncontrolled group is significantly lower to be ultimately recognized as a treatment method. Among the subjects, the proportion of those educated through public health centers and clinics is relatively low. Of course, it is necessary to access the knowledge of diabetes through diverse channels, yet it is necessary to expand the base so that education can be conducted in institution where mediation can be more professional and tailored to the health condition, characteristics, and needs of the individual.
Although our research is representative sample data of the people as a national health and nutrition survey data, it has limitations that an error in sampling rate may have occurred due to cross-sectional study at a certain time of investigation, and that it may contain errors such as response bias. The relevance of various factors, such as glucose control and educational performance, can be found, but it is difficult to clearly identify causal relationship. Moreover, due to the old data, it does not reflect the recent trends. This is because many variables related to diabetes were excluded after the fifth data of the Korea National Health and Nutrition Examination Survey. However, it can still be meaningful that many factors such as socio-economic indicators and lifestyles were combined and that the analysis of a large number of people was conducted.
CONCLUSION
Diabetes patients are steadily increasing, so several national management plans are being pursued, but policies including the cost of educations have not been continuously improved. Based on this study, it is necessary to standardize education management and improve the level of educators and programs for diabetes. We think that the education performance rate of diabetes should be increased by providing various educational institutions with convenient access. Finally, various national survey should be resumed, and multidisciplinary studies on the educational effects should be attempted.
NOTES
-
Conflict of Interest: The authors declare that they have no competing interests.
REFERENCES
- 1. Blaslov K, Naranđa FS, Kruljac I, Renar IP. Treatment approach to type 2 diabetes: past, present and future. World J Diabetes 2018;9:209-219.
- 2. Melmer A, Laimer M. Treatment goals in diabetes. Endocr Dev 2016;31:1-27.
- 3. Nathan DM. Diabetes: advances in diagnosis and treatment. JAMA 2015;314:1052-1062.
- 4. Świątoniowska N, Sarzyńska K, Szymańska-Chabowska A, Jankowska-Polańska B. The role of education in type 2 diabetes treatment. Diabetes Res Clin Pract 2019;151:237-246.
- 5. Chatterjee S, Davies MJ, Heller S, Speight J, Snoek FJ, Khunti K. Diabetes structured self-management education programmes: a narrative review and current innovations. Lancet Diabetes Endocrinol 2018;6:130-142.
- 6. McElfish PA, Long CR, Bursac Z, Scott AJ, Felix HC, Schulz TK, Worley MA, Rowland B. Diabetes self-management education exposure and glycated haemoglobin levels among Marshallese participants in a randomized controlled study. Diabet Med 2020;37:319-325.
- 7. Duncan I, Ahmed T, Li QE, Stetson B, Ruggiero L, Burton K, Rosenthal D, Fitzner K. Assessing the value of the diabetes educator. Diabetes Educ 2011;37:638-657.
- 8. Kim JH, Chang SA. Effect of diabetes education program on glycemic control and self management for patients with type 2 diabetes mellitus. Korean Diabetes J 2009;33:518-525.
- 9. Vitale M, Xu C, Lou W, Horodezny S, Dorado L, Sidani S, Shah BR, Gucciardi E. Impact of diabetes education teams in primary care on processes of care indicators. Prim Care Diabetes 2020;14:111-118.
- 10. Fredrix M, Byrne M, Dinneen S, McSharry J. ‘It's an important part, but I am not quite sure that it is working’: educators' perspectives on the implementation of goal-setting within the ‘DAFNE’ diabetes structured education programme. Diabet Med 2019;36:80-87.
- 11. Chawla SP, Kaur S, Bharti A, Garg R, Kaur M, Soin D, Ghosh A, Pal R. Impact of health education on knowledge, attitude, practices and glycemic control in type 2 diabetes mellitus. J Family Med Prim Care 2019;8:261-268.
- 12. Sriphrapradang C, Mongkolrattanakul P, Tanasanitkul H, Reutrakul S. Improving inpatient glycemic control by diabetes education program in internal medicine residents. Diabetes Metab Syndr 2019;13:2647-2652.
- 13. Lee DH, Keum N, Hu FB, Orav EJ, Rimm EB, Willett WC, Giovannucci EL. Comparison of the association of predicted fat mass, body mass index, and other obesity indicators with type 2 diabetes risk: two large prospective studies in US men and women. Eur J Epidemiol 2018;33:1113-1123.
- 14. Møller G, Andersen HK, Snorgaard O. A systematic review and meta-analysis of nutrition therapy compared with dietary advice in patients with type 2 diabetes. Am J Clin Nutr 2017;106:1394-1400.
- 15. Yang D, Yang Y, Li Y, Han R. Physical exercise as therapy for type 2 diabetes mellitus: from mechanism to orientation. Ann Nutr Metab 2019;74:313-321.
- 16. Gohdes D. Diet therapy for minority patients with diabetes. Diabetes Care 1988;11:189-191.
- 17. Ewers B, Bruun JM, Vilsbøll T. Effects of basic carbohydrate counting versus standard outpatient nutritional education (the BCC study): study protocol for a randomised, parallel open-label, intervention study focusing on HbA1c and glucose variability in patients with type 2 diabetes. BMJ Open 2019;9:e032893.
- 18. Ahmadzadeh Tori N, Shojaeizadeh D, Sum S, Hajian K. Effect of BASNEF-based nutrition education on nutritional behaviors among elderly people and Mini Nutritional Assessment on nutritional status in elderly with diabetes with type 2 diabetes (a clinical trial intervention). J Educ Health Promot 2019;8:94.
- 19. Tan E, Khoo J, Gani LU, Malakar RD, Tay TL, Tirukonda PS, Kam JW, Tin AS, Tang TY. Effect of multidisciplinary intensive targeted care in improving diabetes mellitus outcomes: a randomized controlled pilot study - the Integrated Diabetes Education, Awareness and Lifestyle modification in Singapore (IDEALS) Program. Trials 2019;20:549.
- 20. Norris SL, Lau J, Smith SJ, Schmid CH, Engelgau MM. Self-management education for adults with type 2 diabetes: a meta-analysis of the effect on glycemic control. Diabetes Care 2002;25:1159-1171.
- 21. Kim Y, Jo Y, Choo H, Han E, Kim C. Effects of a self-control promotion program on self-efficacy, selfcare and physiological indicators of patients with diabetes living in local communities. J Korean Acad Rural Health Nurs 2010;5:5-15.